Let’s start with a story: the case of a young patient.
A customer of 36-year-old woman banking professional was told her that there was a swelling in her neck that became prominent whenever she looked up from her desk. Could it be a thyroid issue? She had not noticed it before, nor had she experienced any symptoms or pain. Therefore, she chose to ignore it as she was busy with work.
After a few days however, she noticed that she had a slight hand tremor while typing and her co-workers often joked about her ‘weight loss strategy’. She discreetly consulted a schoolfriend, who was a doctor. Her doctor friend informed her that she probably had a thyroid disorder, hyperthyroidism. She then underwent a battery of lab tests and scans and was prescribed medications. Although she was comfortable for a few weeks, her symptoms recurred. When the dosage of her medication was increased, she felt sick and developed skin rashes. Next, she was guided to a senior thyroid surgeon, who offered her two choices: surgery for the thyroid disorder or radioactive iodine treatment. Both terms frightened her. The thought of surgery was stressful enough—but “radioactive”? That word made her anxious, and suddenly, all her dreams of her future crashed.
This time, her schoolfriend doctor personally accompanied her to the Nuclear Medicine Department of a hospital and arranged a consultation with the specialist. The nuclear physician performed another scan to confirm hyperthyroidism: to check that her thyroid gland was indeed overactive, and that she would respond well to radioactive iodine. She came back the following week to swallow a capsule containing radioactive iodine and was prescribed a few other medications. Her symptoms gradually subsided over the next few weeks, and her medications were gradually tapered off. She is now closely monitoring her weight and follows-up regularly with her doctor.

Iodine and its use in our body
What is radioactive iodine? What role does iodine play in our body?
Iodine is an important micronutrient for the human body and is present in minute quantities in everyone, with about 10 micrograms of iodine in 100 ml of blood — about 18 mg in the entire body. We derive our daily iodine requirement from the food we eat, water we drink and the air we breathe. Adults require 150 micrograms per day. Pregnant women and nursing mothers require about 300 micrograms while children may require about 120 micrograms per day. More than 80% of this iodine is trapped in the thyroid gland and helps in the synthesis of complex hormones such as thyroxine as well as amino acids, which are essential for normal metabolism. The body excretes unutilised iodine predominantly through urine — normally about 200 micrograms/litre of urine.
The World Health Organization (WHO) defines iodine deficiency as urinary iodine concentration of less than 100 micrograms/litre of urine in an adult while excessive iodine intake is defined as greater than 300 micrograms/litre of urine.
Understanding iodine
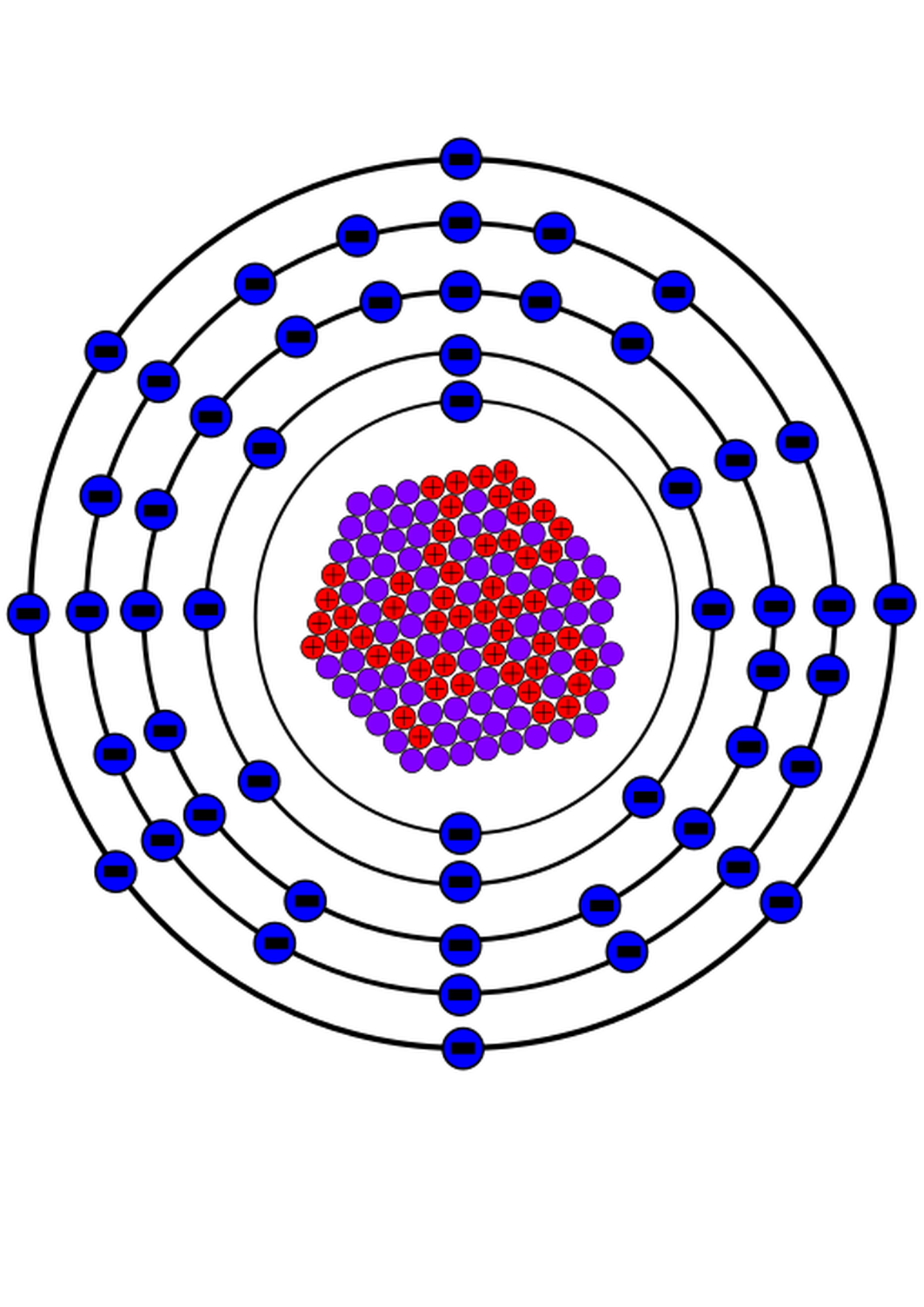
All iodine isotopes contain 52 protons and multiple neutrons in their nucleus. There are about 40 isotopes of iodine produced in laboratories or found in nature, of which 127Iodine (127I) is physically stable and abundant. Except for 127I, all iodine isotopes are man-made, either in nuclear reactors or in particle accelerators called Cyclotrons.
In 1938, Glenn Seaborg and John Livingood at the University of California, Berkeley discovered the radioactive iodine isotope 131I. This isotope has a half-life of about 8 days and is now commonly used in medicine. Only four iodine isotopes: 123I, 124I, 125I and 131I are medically useful, while the rest have only industry and research applications.
Radioactive iodine in medicine
On November 12, 1936, Karl Taylor Compton, president of the Massachusetts Institute of Technology delivered a lecture on the topic ‘What Physics Could do for Biology and Medicine’. Seated in the audience, was then 31-year-old chief of the thyroid clinic at the Massachusetts General Hospital, Saul Hertzcan, who asked “Can iodine be made artificially radioactive?” Although Dr. Compton was initially unsure about how to respond, he made a note of this question and responded positively in a letter on December 15, 1936. This was the beginning of the use of radioactive iodine for hyperthyroidism and thyroid cancer.
The discovery of 131I two years later, began the success story of nuclear medicine. It’s high energy gamma rays help in medical imaging while high energy beta particles help destroying hyperfunctioning thyroid cells. The other three medically-useful iodine isotopes meanwhile, are helpful in imaging thyroid function.
Iodine I31I is used in medicine
| Photo Credit:
By SM358 – Inkspace, Public Domain, https://commons.wikimedia.org/w/index.php?curid=112475552
Today, radioactive iodine therapy is used to treat hyperthyroidism: due to diffuse toxic goitre or toxic multi nodular goitre, or toxic nodules in the thyroid gland. Once a capsule containing a radioactive form of iodine is swallowed, the hyperfunctioning thyroid tissues in the gland absorbs the radioiodine. The radiation emitted can break down complex molecules, supressing the thyroid cells and leading to a decrease in the production of the thyroid hormone, thereby normalising levels. This works like an operation at the molecular level, with gamma radiation allowing doctors to track and measure these changes, known as ‘theranostics’ (therapy + diagnostics). Higher amounts of radioactive iodine are used for ablation of slow-growing and refractory differentiated thyroid cancers.
The Indian scenario
In India, 131I is routinely used only for scanning and treatment purposes. For scanning of benign thyroid disease and goitres, radioactive technetium pertechnetate (99mTcO4) is used because it has a very short half-life (about six hours only) and gives better functional images. For treatment of hyperthyroidism, a small quantity of 131I (about 370 MBq to 740 MBq) is administered orally as a capsule or drunk in a liquid form – sodium iodide oral solution.
For thyroid malignancies, very tiny quantities of 131I (amounting to 37 to 74 MBq) are used for whole body scanning of patients who have undergone surgery for total removal of the thyroid gland to evaluate for residual tissue and metastasis. For ablation of remnant thyroid tissue and metastatic tissues, larger doses (about 2.5GBq to 5.6 GBq) of 131I are administered after careful preparation. Patients are monitored by a specialised team of experts under the supervision of a Level 3 Radiological Safety Officer and admitted in special wards. They remain in these wards with appropriate radiation protection until the level of radiation emitted from them decreases to less than 50 micro Sv per hour, in accordance with regulatory norms in India. Subsequent to their discharge, they follow certain safety practices for 110 days to reduce the radiation exposure to their families. Handling and administration of radioactive iodine or any radioactive medication is strictly regulated and monitored.
Pregnancy is the absolute contraindication for radioactive iodine treatment. Any treatment with radioactive medications is not given to pregnant women and nursing mothers. Therefore, all women of reproductive age are carefully screened for pregnancy before administration of radioactive iodine.
Patients may experience dryness of mouth/acidity/dyspepsia/nausea/dry eyes/skin itching or headache for a few days. Such symptoms can be managed with simple medications given at the time of discharge. They are encouraged to drink adequate water and take sour lozenges to enhance salivary secretion.
All patients are followed up every six to eight weeks after their treatment by monitoring their thyroid hormone levels and significant weight changes. In patents who have undergone treatment for thyroid cancers, their thyroid hormone levels are maintained slightly above the physiologically acceptable levels to prevent recurrence of metastatic disease.
Hope for many
Circling back to the story we began with: the patient is still being monitored by her doctor, over 10 years later. She has been taking a minimal dose of thyroxine for past five years because her thyroid gland has now become slightly underactive. Her health is back to normal, she is scar-free, happy and productive.
(Dr. E. Prabhu is president, Society of Nuclear Medicine India. dreprabhu@gmail.com. Dr. M. S. Senthil Kumar is president, Thyroid Federation of India. medisen@gmail.com)
Published – July 19, 2025 10:29 am IST

