Uterine fibroid prevalence in India varies across studies, with some reporting rates between 20% and 40% in women of reproductive age, while others show higher percentages, even up to 77% developing fibroids during their childbearing years. While there isn’t a specific national health programme in India directly targeting uterine fibroids, they are addressed within the broader framework of reproductive health and maternal care programmes.
As the world observes Fibroid Awareness Month this July, clinicians and public health professionals in India are drawing attention to how uterine fibroids — non-cancerous tumours of the uterus that while not life-threatening, can severely affect a woman’s quality of life, especially when symptoms are left unaddressed or misunderstood.
Understanding fibroids
“Fibroids are growths arising from the muscle wall of the uterus. They are not cancerous,” explains A. Jaishree Gajaraj, head of obstetrics and gynaecology at MGM Healthcare, Chennai. “They are fairly common. Across all age groups, 5 to 6 out of 10 women may have fibroids, with peak occurrence in the late 30s and 40s.”
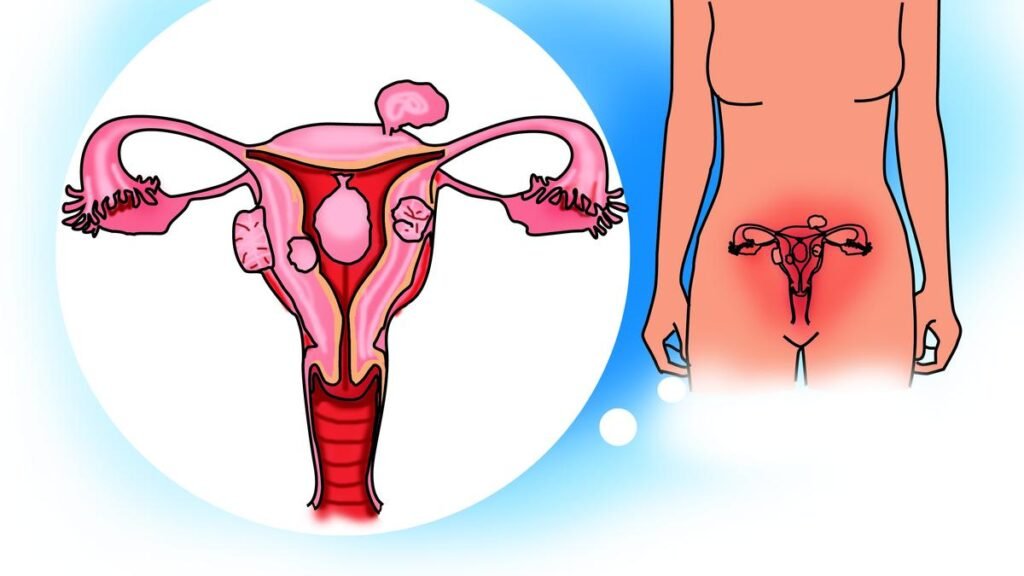
Uterine fibroids, also known as leiomyomas or myomas, are noncancerous (benign) tumors that develop in the uterus. They are the most common type of growth found in a woman’s pelvis and are typically not cancerous. These tumors can vary in size, from as small as an apple seed to as large as a grapefruit, and can grow in different locations within or on the uterus
| Photo Credit:
Special Arrangement
Also known as leiomyomas, fibroids are the most common benign tumours in women. Their presentation varies widely from a single asymptomatic growth detected incidentally on an ultrasound, to multiple large fibroids causing severe pain and bleeding.
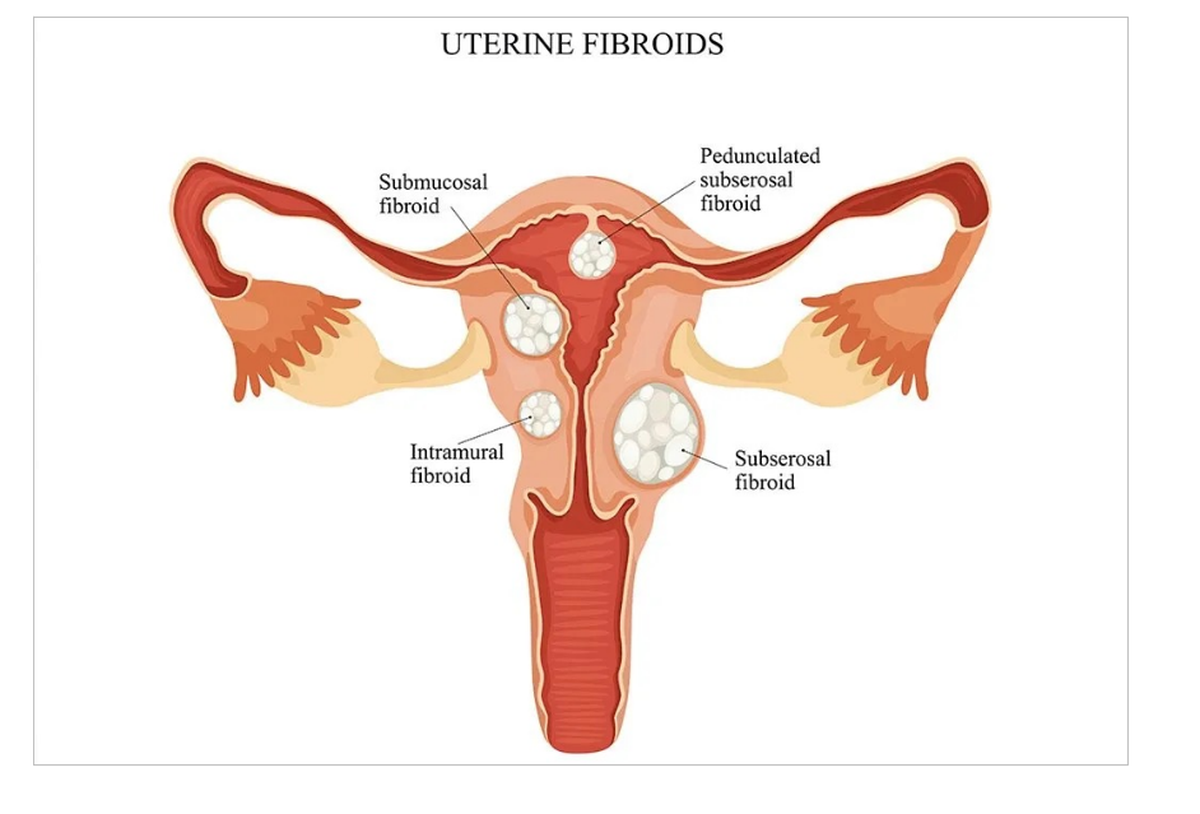
Fibroids are classified based on location — intramural (within the uterine wall), submucosal (into the cavity) and subserosal (towards the outer surface). Submucosal fibroids are more likely to cause heavy bleeding and fertility issues, while subserosal ones are typically associated with pressure symptoms.
Symptoms and consequences of delay
While many fibroids are asymptomatic, a sizeable number of women experience distressing symptoms such as heavy and prolonged menstrual bleeding, pelvic pain, bloating and fatigue. Depending on their location, fibroids can also exert pressure on adjacent organs, leading to urinary frequency, bowel irregularities, and in some cases, difficulty in conceiving or carrying a pregnancy to term.
“The symptom depends on the size and site of the fibroid,” says Dhivya Sharona, consultant, obstetrics and gynaecology, Rela Hospital, Chennai. “Anterior fibroids can cause urinary issues, while posterior ones may result in constipation and pelvic pressure that radiates to the back and legs.”
Short-term consequences include anaemia, fatigue, and reduced work capacity. Long-term effects, if untreated, may range from reproductive complications to chronic discomfort and repeated surgical interventions. In rare cases, fibroids may undergo degeneration or, very rarely, progress to leiomyosarcoma, a malignant variant seen in 0.4 to 0.5% of cases.

A spectrum of treatment pathways
Management of fibroids is highly individualised and depends on the woman’s age, severity of symptoms, fibroid size and location, and her reproductive plans. “Need for future childbearing is an important factor in decision-making,” says Dr. Gajaraj. “Medical management focuses on controlling bleeding and pain. Surgery is considered when symptoms are significant.”
Small, asymptomatic fibroids often require no immediate treatment, with periodic follow-up and ultrasound monitoring. For women nearing menopause, medical therapy may suffice, as fibroids tend to regress after hormonal changes associated with menopause. Hormonal therapy, including the levonorgestrel intrauterine system (LNG-IUS), is commonly used to control bleeding and reduce fibroid volume.
Surgical interventions remain standard for moderate to large fibroids, or when medical therapy is ineffective. These include myomectomy — either open or laparoscopic for uterus-sparing fibroid removal, and hysterectomy for women who have completed childbearing. Minimally invasive procedures such as hysteroscopic resection are offered when fibroids are within the uterine cavity.
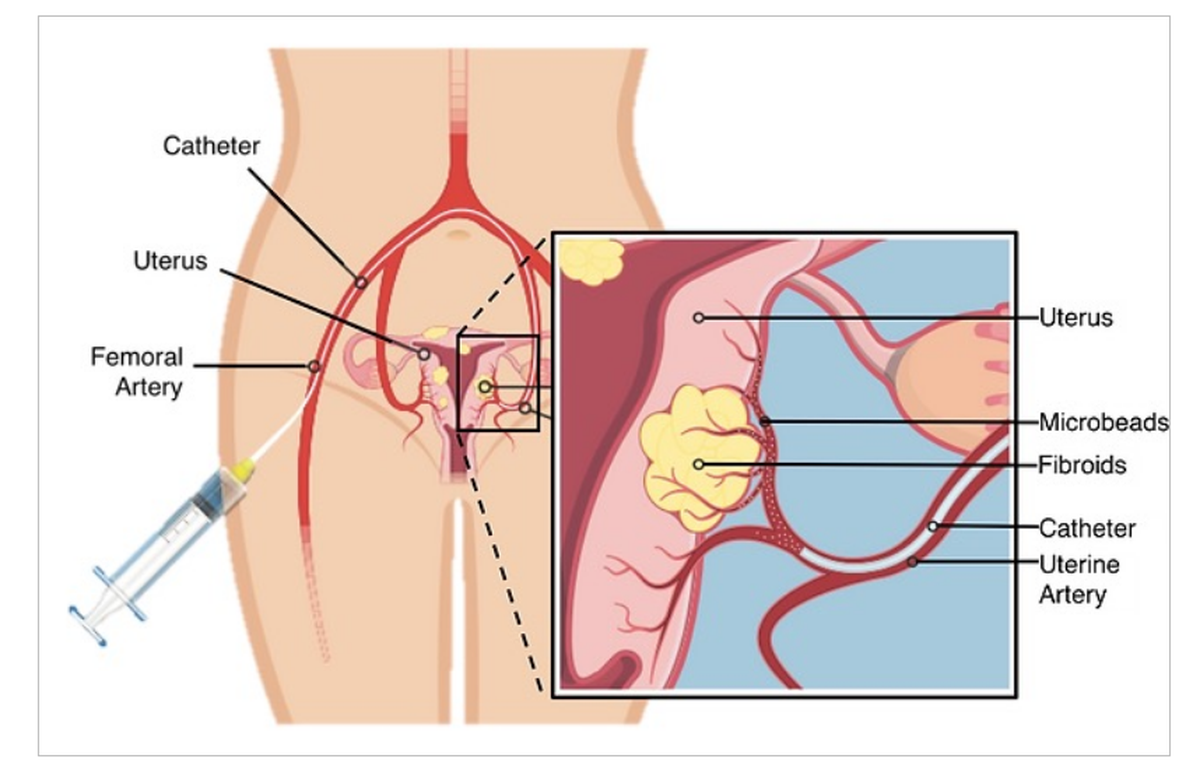
Among the newer non-surgical options is Uterine Fibroid Embolisation (UFE), a minimally invasive image-guided procedure that offers an alternative to traditional surgery. “UFE involves guiding a catheter to the uterine arteries and injecting particles to block blood supply to the fibroids,” explains Basavaraj Biradar, consultant, interventional radiologist at Narayana Health, Bengaluru. “This causes the fibroids to shrink over time, significantly reducing symptoms. Most patients return to normal activities within a week.”
Despite over two decades of global use and recognition by the American College of Obstetricians and Gynecologists (ACOG), awareness about UFE in India remains limited. “Most women have never heard of it,” says Dr. Biradar. “It is essential that all treatment options, including UFE, are discussed with patients.”

Access, awareness and the role of primary care
As treatment options expand from conventional surgery to hormone therapies, minimally invasive techniques, and interventional radiology the need for timely diagnosis and patient-centred care has never been more pressing. “Treatment should be individualised, but access should be universal,” says Dr. Sharona.
Socio-economic and cultural factors continue to influence fibroid diagnosis and treatment in India. Women from lower-income groups often face delayed diagnosis due to limited access to healthcare and lack of awareness about menstrual abnormalities. “Socio-economic background may delay access but doesn’t change the approach to treatment,” says Dr. Gajaraj.
Early diagnosis remains a challenge in India, particularly due to the asymptomatic nature of many cases. “A significant number of women only seek care when symptoms become unmanageable,” says Dheeraj Tiwari, head of interventional radiology at Narayana Health City, Bengaluru. “We should aim to bridge this gap through targeted screening camps and community outreach, which help identify fibroids at an earlier, more manageable stage.” He also emphasises the role of patient counselling in improving uptake of less invasive treatments such as UFE, especially among women hesitant about surgery.
Mannan Gupta, chairman and head of obstetrics and gynaecology at Elantis Healthcare, New Delhi, says: “Fibroids are present in almost 25–30% of Indian women, but many remain undiagnosed due to low symptom recognition or lack of access,” he says. “Women from lower socio-economic backgrounds often suffer longer before seeking help, and by then, treatment options may become more invasive. This makes education, both at the primary care level and among the public, absolutely critical.”
Additionally, cultural sensitivities and social beliefs also influence treatment choices, particularly when discussing options like hysterectomy. “Informed and personalised decision-making is key,” says Dr. Sharona. “The patient’s belief systems and family situation must be taken into account.”
Primary care physicians must play a central role, say experts. “They are the first point of contact and often enjoy the trust of patients and their families,” says Dr. Gajaraj. “Education on menstrual health and early referral to specialists can make a significant difference.”
Uterine fibroid treatments vary based on symptom severity and individual patient needs. Watchful waiting with lifestyle adjustments may be sufficient for mild or asymptomatic cases. Medications like hormonal therapies (birth control pills, GnRH agonists) and pain relievers can help manage symptoms. Surgical options, such as myomectomy (fibroid removal) or hysterectomy (uterus removal), are available for larger or symptomatic fibroids. Additionally, minimally invasive procedures like uterine artery embolisation and MRI-guided focused ultrasound offer alternative treatment approaches
| Photo Credit:
Special Arrangement
Despite the prevalence of fibroids, there is no national screening programme dedicated to their detection or management. However, tertiary care hospitals and professional bodies such as the Federation of Obstetric and Gynaecological Societies of India (FOGSI) have stepped in with anaemia awareness drives and women’s health camps. These often include routine gynaecological evaluations and ultrasound screenings that help identify fibroids early.
Experts say that fibroid awareness month should be a call to action for healthcare systems to prioritise early intervention to ensure that every individual has access to informed appropriate and compassionate care.