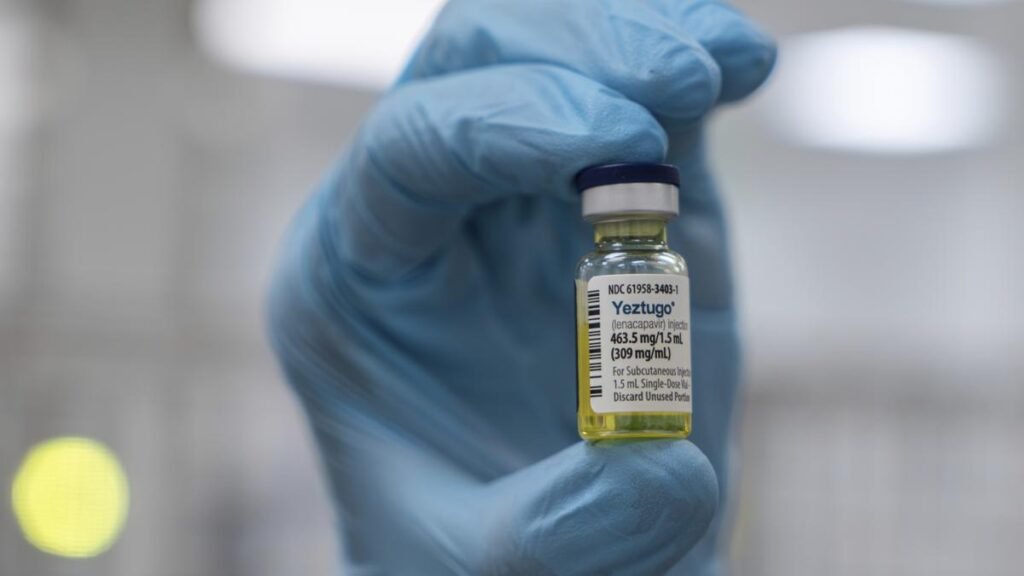
On July 25, The European Medicines Agency (EMA)’s advisory committee recommended Gilead Sciences’ Lenacapavir, a twice-yearly injection, for preventing HIV infection in adults and adolescents. Any recommendation by EMA’s advisory committee has to be formally approved by the European Commission, which is expected later this year. The recommendation by the EMA’s advisory committee comes about a month after the U.S. FDA on June 18, 2025 approved the injectable HIV-1 capsid inhibitor as a pre-exposure prophylaxis (PrEP).
The World Health Organization welcomed the approval by FDA on June 19 and issued guidelines for use of Lenacapavir for HIV prevention on July 14. “Offering additional pre-exposure prophylaxis (PrEP) choices has the potential to increase uptake and effective use of PrEP, and of HIV prevention overall, as it allows people to choose a method that they prefer,” the guidelines say. Studies have also shown that Lenacapavir can achieve significant viral suppression, even in cases where other drugs have failed.
The FDA approved Lenacapavir is based on the 2024 results from the PURPOSE 1 and PURPOSE 2 trials, which demonstrated the safety and efficacy of the pre-exposure prophylaxis injectable across diverse populations and settings. The PURPOSE 1 was a Phase 3, double-blind, randomised trial to evaluate the safety and efficacy of twice-yearly, subcutaneous Lenacapavir for pre-exposure prophylaxis (PrEP) and was tested on 5,338 cisgender women and adolescent girls aged 16-25 across 25 sites in South Africa and three sites in Uganda. The injectable was compared with an active control arm that received once-daily oral pre-exposure prophylaxis drug Truvada (emtricitabine-tenofovir disoproxil fumarate; F/TDF). There were zero HIV infections among 2,134 participants in the Lenacapavir group, while the active control group had 39 infections among 2,136 participants.
In the PURPOSE 2 Phase-3 trial involving 3,265 participants in the modified intention-to-treat analysis, two participants were infected with HIV in the arm that received the injectable, while nine participants who received the active control PrEP oral drug Truvada (emtricitabine-tenofovir disoproxil fumarate; F/TDF) were infected. The background HIV incidence in the screened population (4,634 participants) was 2.37 per 100 person-years. The trial was carried out in of cisgender men, transgender, and nonbinary individuals across 88 sites in Argentina, Brazil, Mexico, Peru, South Africa, Thailand and the U.S.
Compared with the generic PrEP oral drug Truvada, which is extremely inexpensive and widely available, Lenacapavir costs $28,000 for two injections. Why would people ever prefer to use Lenacapavir considering the cost? “Oral PrEP will be effective only if there is 100% adherence. The oral drug won’t work even if it is missed for a day because the drug level will be only 24 hours,” says Dr. N. Kumarasamy, Chief and Director, VHS-Infectious Diseases Medical Centre, Voluntary Health Services, Chennai.
“People who have the highest risk such as sex workers and gay men have to take the drug every day. Taking a tablet every day, even for a deceased patient, is so difficult. They tend to miss a dose, which is why adherence is never 100%,” he says. “Even in the case of on-demand PrEP, where people who want to indulge in unprotected sex have to take the oral drug two days before, then throughout the period of risky behaviour and continue for two more days after risky behaviour ends, adherence never goes beyond 85-90%. PrEP will work only if the adherence is 100%.”
According to Dr. Kumarasamy, despite the oral tablet being inexpensive and easy to take, the adherence is less than ideal, the reason why people are moving towards long-acting injectables that prevent HIV infection for months after an injection. Cabotegravir, which was developed as pre-exposure prophylaxis (PrEP), underwent trials in many countries and was approved for use. Cabotegravir, which is administered intramuscularly every two months, was found superior compared with every day oral PrEP tablet, and started getting implemented in certain parts of the world, Dr. Kumarasamy says.
“Since Cabotegravir has to be administered every two months, people tend to forget. The new drug Lanacapivir has been found to be effective for six months in the trials. The injectable was developed in 2021 as treatment in people who no longer respond to other drugs as they have developed resistance,” he says.
Because Lenacapavir was found to be long-acting, it was repurposed as a pre-exposure prophylaxis administered subcutaneously. “Lenacapavir is a robust molecule and is the best solution in the absence of vaccines. Even if there is going to be an HIV vaccine one day, I’m sure people will have to take the vaccine every year or something. Like a flu shot, you know if at all they are going to develop a vaccine, people may have to take it every year or every six months as a booster dose. It may not be like a one dose that is effective for years,” Dr. Kumarasamy says. “In the absence of a HIV vaccine, I think the pre-exposure prophylaxis every six months can be considered like a vaccine.”
Gilead is developing the same molecule to be administered once a year instead of every six months. They are already working on that. But it will not be a subcutaneous form but as an intramuscular injection, he says.
Licensing agreements
On October 2, 2024, Gilead Sciences signed non-exclusive, royalty-free voluntary licensing agreements with six pharmaceutical manufacturers to make and sell generic Lenacapavir. Of the six generic manufacturers, four are in India. Besides signing agreement to license generic manufacturers to make the injectable, Gilead Sciences also said that it would “support low-cost access to the drug in high-incidence, resource-limited countries at no profit until generic manufacturers are able to fully support demand”. These countries are: Botswana, Eswatini, Ethiopia, Kenya, Lesotho, Malawi, Mozambique, Namibia, Nigeria, Philippines, Rwanda, South Africa, Tanzania, Thailand, Uganda, Vietnam, Zambia and Zimbabwe.
The company has licensed Dr. Reddy’s Laboratories Limited, Emcure, Hetero and Mylan, a subsidiary of Viatris, to manufacture Lenacapavir in India. The companies will be permitted to supply to 120 countries. According to the press release, the agreements cover not only Lenacapavir for HIV prevention but also for HIV treatment in heavily treatment-experienced (HTE) adults with multi-drug resistant HIV.
According to Dr. Kumarasamy one company has already started developing the drug and Lenacapavir may become available next year once the Indian drug regulator approves it based on the results of a safety study carried out in India. As per his estimate, the generic form of Lenacapavir will cost about $100 per dose.
Published – July 27, 2025 03:10 pm IST